Rethinking care at end of life: The Compassionate Communities Connectors Program
An article written by Professor Samar Aoun
The Compassionate Communities model of palliative and end-of-life care emphasises the central role of community development and consumer engagement in partnership with health services in the delivery of care. This approach actively involves a range of stakeholders (including neighbourhoods, workplaces, schools, service clubs, local government and places of worship), to facilitate community networks that can support those experiencing death, dying, grief, and loss.
In the South West of Western Australia, the Compassionate Communities Connectors program has been developed and implemented by the South West Compassionate Communities Network in partnership with WA Country Health Service care teams (2020-22). Community volunteers (known as “Connectors”) were trained to enlist helpers from the community (known as Caring Helpers) to enhance supportive networks that can provide practical and social support to people with advanced chronic conditions and/or life-limiting illnesses.
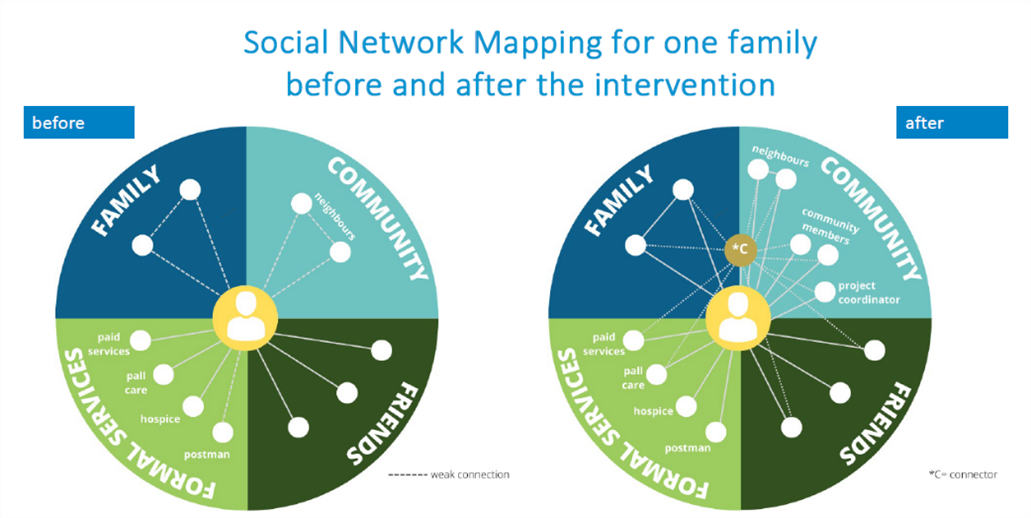
Evaluation of the program showed significant improvements in the social connectedness of supported families, reflected in reduced social isolation, better functioning with daily activities, and a two-fold increase in supportive networks. [1]
For the Connectors, volunteering within this model of care has been a rewarding and feasible experience for nurturing a sense of community among participants, developing relationships with other community members, and seeing the difference that the Connector role makes in the lives of those involved in the enhanced network and fostering growth in Connectors’ emotional capacity and compassion. [2]
Families greatly appreciated the support and enablement received from Connectors, were grateful to have someone outside the family who was knowledgeable and supportive that they could turn to, for relationship building and reducing their social isolation, and regaining control over their situation. [3]
Healthcare providers were impressed with the high level of resourcefulness exhibited by Connectors and perceived a great need for the program, particularly for those socially isolated. They reported increased capacity of their service to provide good care, and that their own practice was enhanced when they started encouraging their clients to ask their social networks for support. [3] The figure below demonstrates the increase in connections for one family, before and after the intervention by the Connectors.
The effectiveness analysis demonstrated significant declines in the frequency of hospitalisations per month and the number of hospital days per month for those in the intervention (“Connector”) group relative to the control population. In contrast, the frequency of outpatient events overall was significantly higher for the intervention group, suggesting that the Connector program has shifted individuals away from the hospital system and back towards community-based care. A cost-consequence analysis assessed the overall economic impacts, indicating a net saving of using the Connector program was $AUD561,256 assuming the enrolment of 100 people with life-limiting illnesses over a 6-month period (forthcoming publication).
Apart from the social and economic benefits, this program has demonstrated a successful partnership between formal health service and informal community networks to foster a more sustainable and affordable approach to care. The program has been integrated into the practice of the health service, an example of a rapid translation, with interest for the program to be replicated in several communities, statewide and nationwide. Findings support the potential benefits of uptake of public health approaches to managing life-limiting disease, with a greater emphasis on partnerships between health services, civic institutions, and communities.
Further information
To learn more, you can view Compassionate Connectors Project 2021, a video showing Connectors in action.
References
- Aoun SM, Richmond R, Gunton K, Noonan K, Abel J, Rumbold B. The Compassionate Communities Connectors model for end-of-life care: implementation and evaluation. Palliat Care Soc Pract. 2022 Nov 30;16:26323524221139655. doi: 10.1177/26323524221139655.
- Aoun SM, Richmond R, Noonan K, Gunton K, Rumbold B. 'The more you give, the better it is for you. You know the reward is greater than the effort': the Compassionate Communities Connectors' experience. Palliat Care Soc Pract. 2022 Nov 30;16:26323524221139874. doi: 10.1177/26323524221139874.
- Aoun SM, Rosenberg J, Richmond R, Rumbold B. The Compassionate Communities Connectors programme: experiences of supported families and referring healthcare providers. Palliat Care Soc Pract. 2023 May 12;17:26323524231173705. doi: 10.1177/26323524231173705.

Professor Samar Aoun
Perron Institute Research Chair in Palliative Care, University of Western Australia.
Chair, South West Compassionate Communities Network
2023 WA Australian of the Year