Centre of Research Excellence in End-of-Life Care (CRE-ELC)
A blog post written by Professor Patsy Yates, Centre Director, NHMRC Centre of Research Excellence in End-of-life Care, Head, School of Nursing, Faculty of Health, Queensland University of Technology; Director, Centre for Palliative Care Research and Education
The pattern of disease, dying and death has changed dramatically in Australia over the last century. In Australia alone almost 160,000 people die every year. Of these at least 120,000 are expected deaths, meaning that access to palliative care could be of great benefit to both the individuals and their families. But ensuring access to quality palliative care for all who need it is not without its challenges. This is why a group of researchers sought funding from National Health and Medical Research Council (NHMRC) for the Centre of Research Excellence in End-of-Life Care (CRE-ELC).
The CRE-ELC brings together four leading research centres in end-of-life care and establishes strategic links with leading investigators in chronic disease, health economics and legal and ethical issues. The chief investigators are based at Queensland University of Technology, The University of Queensland, Flinders University and University of Wollongong. The CRE-ELC is focused on generating the evidence required to ensure end-of-life services are responsive to the complex, unpredictable and often extended patterns of disease progression that characterise end-of-life trajectories for many people today.
The CRE-ELC has three programs of research activity that are aligned with national priorities.
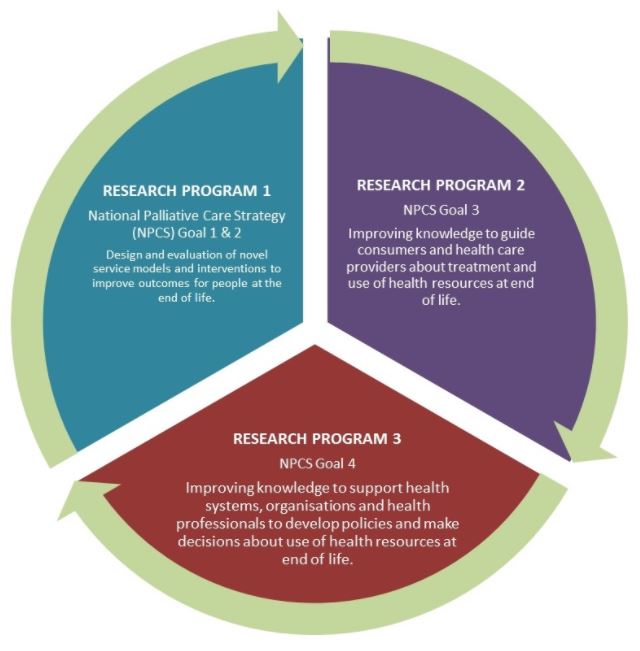
In Stream 1, our primary objective is to identify service delivery models that will achieve best outcomes for various end-of-life populations. For example, we have completed a study focused on understanding the health service needs of people with Stage 3-5 chronic kidney disease (CKD). The study involved following patients with advanced and progressive CKD for 12 months to collect their symptom experience, quality of life, supportive care needs and health service utilisation during that period. The most prevalent symptoms reported were pain, fatigue and breathlessness while sexual and sleep problems were the most troublesome (Bonner et al. 2018). Patients were also found to be frequent users of acute health services (Chambers et al. 2018 In Press).
Other projects completed within this stream have focused on understanding how we can reform primary care services at end-of-life. The BASIC-NP Project involved development and evaluation of an integrated palliative nurse practitioner (NP) service. This study identified that NP-coordinated, GP-supported care resulted in prompt instigation of end-of-life care, appropriate follow up, and a comprehensive care plan (Mitchell et al, 2016). A second study examined integrated care approaches to end of life in the primary care setting; these were confirmed by a sample of GPs we interviewed to be most effective. Not surprisingly, effective communication between members of multidisciplinary teams was key to successful care (Rosenberg, 2017). Following these studies, further work was undertaken, including a design-thinking workshop to provide a forum for various stakeholders to create new solutions to address the challenges associated with GP involvement in palliative care. The innovative methodology underpinning this work enabled the 23 expert participants to identify five key challenges: integrated care; community awareness; early identification and planning; data on quality of care; and funding models. Workshop findings will be communicated in more detail once the manuscript is finalised and published.
Our consumer stream (Stream 2) is focused on understanding what can be done to ensure palliative care services are centred on consumer needs, with the goal to ensure collaborative decision making processes at end of life. As part of this stream, we are currently undertaking a systematic review to identify the factors that influence consumers’ end-of-life treatment decision making. We have also developed a proposal for a pilot project aimed at developing tools for measuring patient and family experiences of palliative care.
CRE-ELC investigators are aware that provision of quality palliative care services also requires system and regulatory reform. Stream 3 was designed to address these issues. As part of this, we are undertaking a two stage study concerned with the legal and ethical risk of the provision of pain relief at end of life. Stage 1 comprises a review of publicly available cases involving the provision of palliative medication that may have resulted in death. Stage 2 involved interviewing nurses caring for patients at end of life – the analysis of which is currently being finalised.
The CRE-ELC is also building capacity in the sector by developing a multidisciplinary research workforce in end-of-life services through collaboration, training of new researchers and developing the next generation of research leaders in end-of-life care. As part of our capacity building strategies, the CRE-ELC has funded top-up scholarships for 6 PhD students. One of these students, whose thesis concerned identifying patients with a haematological malignancy at high risk of deteriorating and dying and who is likely to benefit from integration of palliative care, has been awarded her PhD. Other students are currently undertaking projects focused on legal aspects of end-of-life services, paediatric palliative care services, and end-of-life decision making.
The establishment of the CRE-ELC has provided an opportunity for researchers from a range of disciplines and sectors to collaborate and develop solutions to some of the major challenges we face with palliative care service provision. Dying may be unavoidable, but I’m proud of the work we are doing to ensure those who need palliative care are getting the highest quality research-based health service interventions. I am also excited by the opportunities the CRE-ELC has provided to apply innovative methodological approaches to transform thinking about the way in which we deliver these necessary services.
References:
Bonner, A., Chambers, S., Healy, H., Hoy, W.E., Mitchell, G., Kark, A., Ratanjee, S., & Yates, P. (2018). Tracking patients with advanced kidney disease in last 12 months of life. Journal of Renal Care, [Epub] DOI:10.1111/jorc.12239.
Chambers, S., Healy, H., Hoy, W.E., Kark, A., Ratanjee, s., Mitchell, G., Douglas, C., Yates, P. & Bonner, A. (2018). Health service utilisation during the last year of life: A prospective, longitudinal study of the pathways of patients with chronic kidney disease stages 3-5. BMC Palliative Care, Accepted with Minor Revisions, currently under final review.
Mitchell, G.K., Senior, H.E., Bibo, M.P., Makoni, B., Young, N.S., Rosenberg, J.P. & Yates, P. (2016). Evaluation of a pilot of nurse practitioner-led, GP supported rural palliative care provision. BMC Palliative Care. 15:93. doi:10.1186/s12904-016-0163-y
Rosenberg, J. (2017). Working in multidisciplinary teams: Understanding GP clinical practice in the end of life care [online]. Australian Nursing and Midwifery Journal, 25(6), 39.

Professor Patsy Yates, Centre Director, NHMRC Centre of Research Excellence in End-of-life Care, Head, School of Nursing, Faculty of Health, Queensland University of Technology; Director, Centre for Palliative Care Research and Education